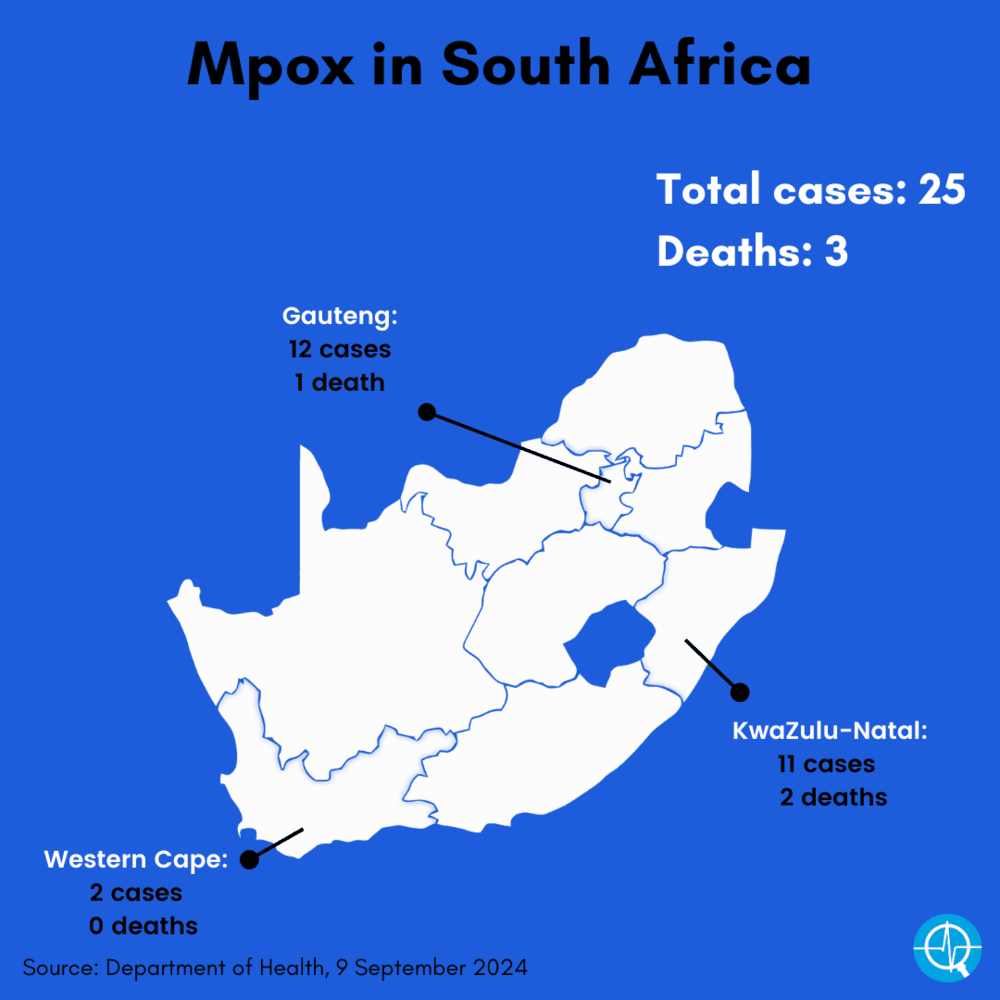
By 9 September, South Africa had 25 laboratory-confirmed mpox cases in three provinces (Gauteng, KwaZulu-Natal and the Western Cape), with three people dying from the virus. (Berkay Ataseven, iStock)

South Africa is one of 14 countries that will be financially supported by the Africa Centres for Disease Control and Prevention (Africa CDC) and World Health Organization (WHO) from this month until February 2025 to draw up and roll out plans, including vaccination strategies, to fight mpox.
The budget for the “mpox continental preparedness and response plan for Africa” is about $600-million of which just over half of the money — 53% — will go towards the mpox responses of 14 of the 55 African Union member states in which cases have escalated, and human-to-human transmission of the monkeypox virus has become relatively common.
In addition to South Africa, the 13 other countries that will be helped to design and roll out plans are: Democratic Republic of Congo (DRC), Burundi, Central African Republic (CAR), Congo, Cameroon, Côte d’Ivoire, Gabon, Liberia, Kenya, Nigeria, Republic of Guinea, Rwanda and Uganda.
Most of the rest of the money — 45% — will be spent on funding the efforts of partners such as Unicef, the International Organisation for Migration and the International Federation of Red Cross, to help countries to set up their plans, become better at testing and contact tracing, managing cases and rolling out vaccines.
The budget for South Africa is $45.5 million (R813 million), of which $10.1 million (R178 667 million) to cover the logistics of rolling out vaccines against mpox. This money can’t be used to buy jabs. The Africa CDC and WHO say vaccines will be funded via in-kind donations and in cases where countries can afford to buy shots, the prices will depend on ongoing negotiations with drugmakers.
In August the WHO declared mpox a public health emergency of international concern, and in the same month the Africa CDC announced it a public health emergency of continental security.
This was the first time that the Africa CDC has made such a declaration since its inception in 2017. The World Health Organisation’s declaration is the second in two years with regards to mpox — in 2022, the WHO also declared mpox a public health emergency of international concern, after a multicountry outbreak, but announced the emergency over in May 2023.
An invitation for vaccine manufacturers to express their interest in listing their anti-mpox shots for emergency use was announced by the WHO on 7 August.
SA now has 25 confirmed mpox cases
Meanwhile, South Africa’s health department announced another mpox case on Monday — a 38-year old man who was diagnosed at a private medical facility in Cape Town — on 6 September.
This brings South Africa’s total number of 2024 cases to 25. Twelve cases were diagnosed in Gauteng, 11 in KwaZulu-Natal and two in the Western Cape. Three have died.
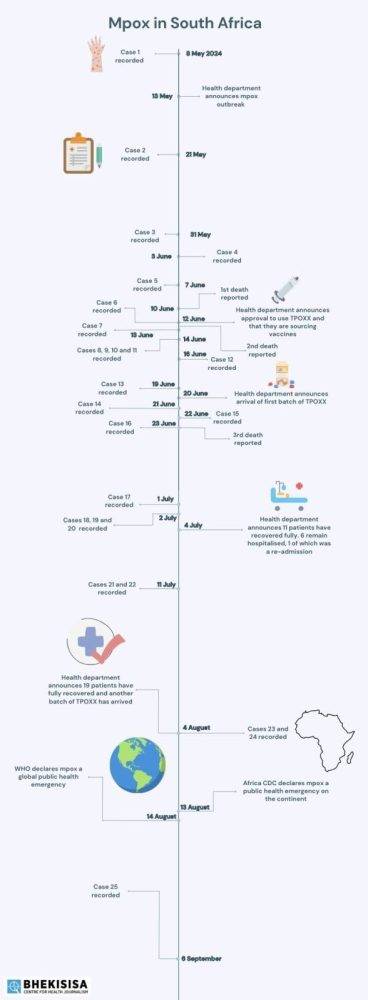
South Africa’s first 2024 case was reported on 8 May.
Where and when were South Africa’s mpox cases diagnosed?
Use our interactive map, created by Bhekisisa’s health reporter, Zano Kunene, to see the details.
]
None of the country’s cases are the relatively new strain, clade 1b, which seems to be deadlier than other forms of the virus. All of South Africa’s cases were infected with clade 2b, the same type of the virus that caused outbreaks in Western Europe and the United Kingdom in 2022 and 2023, according to health department spokesperson Foster Mohale.
Almost all South Africa’s cases were among gay and bisexual men, most in their twenties or thirties, and many of them were infected with HIV, but untreated.
South Africa’s latest case does not have an international travel history and went to the doctor on 4 September after he noticed typical mpox-like blisters on his face, chest and genitals. He wasn’t hospitalised, but is in a stable condition and isolating at home.
The differences between clade 1 and 2
Mpox is caused by the monkeypox virus and there are two known clades: clade 1 and clade 2. Mpox starts off with a fever, muscle aches and a sore throat, followed by blister-like bumps on the skin on any part of the body. Most people recover spontaneously, but people with weakened immune systems, such as those with untreated HIV, often fall very ill with the disease, and some die.
Clade 1 has been rampant in the Democratic Republic of Congo, where mpox has been recorded for over a decade, but in August cases were also detected in Sweden and Thailand. Moreover, from 2023 onwards, clade 1 cases were found in Kenya, Rwanda, Burundi, the Central African Republic and Uganda; all countries close to the DRC. The cases in Sweden and Thailand had both travelled to African countries where clade 1 cases had been detected.
The WHO says clade 1 cases in the DRC have increased steadily over the past decade, especially in 2023. At over 15 600 cases and 537 deaths, the numbers reported so far in 2024 are more than last year’s total.
Clades 1 and 2 cause the same type of disease, but infection with the clade 1 virus makes people feel sicker and can lead to more deaths. Although symptoms of a clade 2 infection are milder, virus of this type spreads easier. Clade 2b cases have mainly spread among gay and bisexual men with HIV, but who are not on treatment, or don’t use their treatment correctly. Clade 1 cases, however, can also spread via children and heterosexual adults who live closely together in a household and may share a bed or linen.
A worldwide vaccine shortage
Last week, the DRC received two shipments from the European Union donation programme of about 100 000 vaccine doses used against mpox each — but it’s not nearly enough. Two such jabs are currently being used globally, both recommended by the WHO’s advisory group on immunisation.
Vaccines specifically against mpox are being developed, but there have not yet been clinical trials that include thousands of people, which is a necessary step in getting any medicine into commercial production.
Although the United States medicines regulator, the Food and Drug Administration, issued an emergency-use licence for a new type of smallpox vaccine to be used against mpox infection in August 2022, in most other places earlier anti-smallpox jabs are used against mpox, because the two diseases are caused by similar-looking viruses.
In South Africa, people were vaccinated against smallpox until the 1980s, when the pandemic was eradicated; those who were vaccinated have about 85% protection against getting infected with mpox.
LISTEN: Mia Malan speaks to the NICD about the mpox outbreak
The health department has previously announced that it will start to vaccinate four groups of people with a higher chance than the general population to contract the monkeypox virus — men who have sex with men, sex workers, health and lab workers — against the monkeypox virus as soon as jabs arrive in the country.
But the department has not yet managed to secure donations.
Mohale says the department has tried to source mpox jabs from Western countries, but “it’s difficult to tell when we can expect the vaccines”. “The department is still considering several options, while at the same time looking at the epidemiological surveillance data.”
With a huge shortage of mpox jabs, the current spread of clade 1 cases is unfolding against the background of vaccine inequity “and yet another looming failure”, experts wrote on 15 August in the British Medical Journal (BMJ).
“We have seen this before, and it does not end well for anyone,” they said.
“Vaccine inequity is already evident”, the BMJ authors wrote, “with Africa CDC reporting a need for approximately 10-million vaccine doses to control the outbreak, of which only about 280 000 are available — less than 3% of the estimated need, even as wealthy countries hoard, stockpile, and refuse to share vaccines.”
The WHO and Africa CDC’s continental plan aims to get 10-million people in Africa vaccinated within the next six months.
The BMJ authors, however, concluded: “Having observed COVID-19 and previous epidemics, we have every reason to worry that high-income nations will make the same mistakes again — from vaccine hoarding to unfair travel bans and anti-Black racism.”
Our health reporter, Zano Kunene, put together a timeline of how mpox has unfolded in South Africa and we’ve added the cases to an interactive map. We’ve also uploaded all the health department’s updates in chronological order, so that you’re able to find all important mpox information in one place.
Mpox in South Africa: 8 May to 9 September 2024
This story was produced by the Bhekisisa Centre for Health Journalism. Sign up for the newsletter.
